A world-first study led by Australian scientists and clinicians has found a way to improve the therapy options, and therefore the survival chances, of children with high-risk cancers. More than 1000 children and adolescents aged 0-19 are diagnosed with cancer each year in Australia, and in those with high-risk cancers, the survival rate is less than 30%.
The study is the first to demonstrate that the practice of pre-clinical testing – developing laboratory models based on each patient’s cancer, then using these models to test potential therapies – significantly increases treatment options for children with high-risk cancer when compared to genetic testing of patient tumours alone.
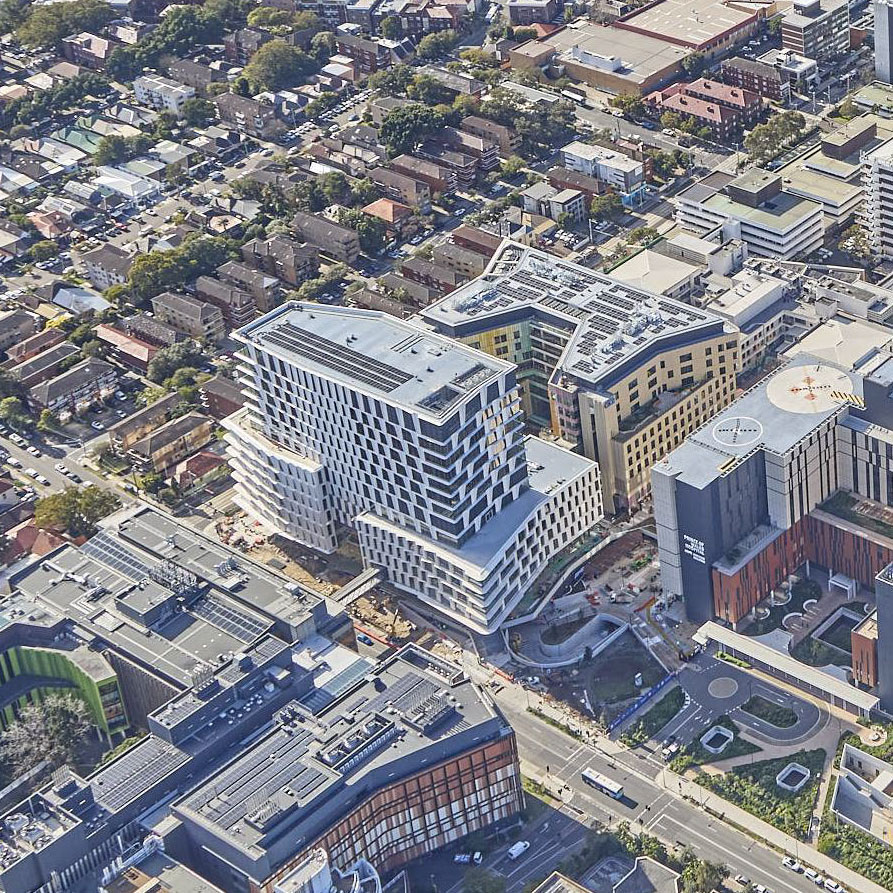
In recent years, the field of personalised medicine has seen treatments matched to individual patients with a precision that has never before been possible, and there is a move worldwide towards using personalised treatment approaches for children with cancer. Australia is home to one of the most comprehensive programs of this kind − the Zero Childhood Cancer Personalised Medicine Program (ZERO), jointly led by Children’s Cancer Institute and the Kids Cancer Centre at Sydney Children’s Hospital, Randwick.
So far, ZERO and other personalised medicine programs for children with cancer have been based on analysing each child’s cancer at a genomic level to find out what is driving the growth of the cancer and how it might best be targeted. This information is then used to provide treatment recommendations to the patient’s oncologist. Using this approach, ZERO has led to some remarkable results over the past six years, and building on this success, the Program is now being progressively expanded to be available to all young people diagnosed with cancer in Australia.
Published this week in the prestigious international medical journal EMBO Molecular Medicine, research by the ZERO team has now shown that personalised medicine results can be significantly improved by adding preclinical testing to the diagnostic platform on which treatment recommendations are based. Using data from 56 children with high-risk cancer enrolled in the ZERO pilot study (TARGET) and treated at Sydney’s two children’s hospitals between 2015 and 2017, the researchers found that pre-clinical testing not only revealed additional drug sensitivities − identifying treatment options in 10 patients that were not identified by genetic testing− but also proved a good predictor of clinical response in patients.
“We were surprised to find that preclinical testing, in many instances, proved even more accurate than molecular analysis in predicting patient response to the recommended therapy,” said Professor Glenn Marshall AM, Clinical Lead of ZERO and co-senior author on the paper. “Adding preclinical testing can therefore not only provide independent proof of drug efficacy suggested by molecular analyses, but also help avoid the use of ineffective treatments.”
Providing such proof may be an important step toward improving the clinical uptake of these treatment recommendations by oncologists, with past research suggesting that insufficient evidence is one of the main reasons oncologists choose not to adopt the treatment recommendations provided for their patients.
One family who has benefited from personalised medicine through the ZERO Program is the Giteau family. Kristy Giteau − a former national women’s rugby player, and sister of ex-Wallaby Matt Giteau − is mother to Ka’ili, a courageous little girl who was diagnosed with a rare kidney cancer in 2019. Treated at the Kids Cancer Centre at Sydney Children’s Hospital, Randwick, Ka’ili initially responded well to therapy, but her cancer grew aggressively, and she relapsed in June 2020. Facing extremely limited treatment options, she joined ZERO. Researchers were able to identify a specific drug that both genetic analysis and preclinical drug testing showed was specifically targeted to her cancer. Her doctors were then able to begin treatment with this drug. Ka’ili is now in remission and doing well.
“I’m so thankful for the world-class treatment Ka’ili received,” said Kristy. “Without ZERO, I dread to think what options we would have been left with. All the testing done on Ka’ili’s cancer led to finding a treatment that worked for her, and I couldn’t be more grateful.”
According to Associate Professor David Ziegler, Clinical Trial Lead for ZERO and co-senior author on the paper, while not every child treated using a personalised medicine approach experiences a positive outcome, future research is likely to lead to further improvements.
“Our research strongly suggests that adding preclinical testing to the diagnostic platform has the potential to improve clinical outcomes for children with high-risk cancer,” he said. “We believe this is a major advance in the field, and one that will provide fresh hope to children with cancer and their families.”
Media contact:
Tania Ewing, 0408 378 422, taniaewing@taniaewing.com
About Zero Childhood Cancer:
The Zero Childhood Cancer Program (ZERO) is a truly collaborative national research and clinical initiative led by Children’s Cancer Institute and Kids Cancer Centre at Sydney Children’s Hospital, Randwick, together with all eight of Australia’s children’s hospitals. The Program is the most exciting childhood cancer research initiative ever undertaken in Australia, and is a huge step towards the ultimate aim which is to see personalised medicine become the new model of care for children and young adults with cancer. For participating hospitals and research centres click here: Participating Hospitals and Medical Research Institutes. ZERO aims to identify the precise make-up of each individual child’s cancer by using sophisticated genomic tests (whole genome sequencing, whole transcriptome sequencing and methylation profiling) to identify the molecular changes (including “mutations”) driving their cancer and matching these with treatments most likely to target their unique cancer. Where possible, preclinical drug testing is carried out to provide further evidence for the most effective treatment. The aim is to identify a personalised treatment plan for each child. ZERO is funded by the Commonwealth Government, Minderoo Foundation and many philanthropic funding partners, for more information click here: ZERO Funding Partners
About Children’s Cancer Institute:
Originally founded by two fathers of children with cancer in 1976, Children’s Cancer Institute is the only independent medical research institute in Australia wholly dedicated to research into the causes, prevention and cure of childhood cancer. Forty years on, our vision is to save the lives of all children with cancer and improve their long-term health, through research. The Institute has grown to now employ over 300 researchers, operational staff and students, and has established a national and international reputation for scientific excellence. Our focus is on translational research, and we have an integrated team of laboratory researchers and clinician scientists who work together in partnership to discover new treatments which can be progressed from the lab bench to the beds of children on wards in our hospitals as quickly as possible. These new treatments are specifically targeting childhood cancers, so we can develop safer and more effective drugs and drug combinations that will minimise side-effects and ultimately give children with cancer the best chance of a cure with the highest possible quality of life. More at www.ccia.org.au
About Kids Cancer Centre, Sydney Children’s Hospital, Randwick
The Kids Cancer Centre (KCC) at Sydney Children’s Hospital, Randwick has been treating children with cancer and blood diseases in NSW, Australia and the Asia-Pacific region for nearly 50 years. Almost two thirds of children treated for cancer or leukaemia at the Centre are enrolled on clinical trials, in a unique model where research and clinical care are one, aimed at ensuring the best possible care for children and their families. During that time the survival rates for children with cancer have gone from 10 per cent to nearly 80 per cent. Clinical and research staff from the Centre have made major international and national contributions to the expansion of knowledge in the area: from important discoveries around bone marrow transplantation, chemotherapy for relapsed solid tumours and leukaemia, to the invention of novel anti-cancer drug combinations and minimal residual disease testing in acute lymphoblastic leukaemia. Centre staff have been leaders in devising new methods of outreach and home nursing, and in developing modern approaches to the bereaved family. These achievements have been founded on academic excellence and clinical expertise. In the past five years alone, Centre staff have published over 200 papers in peer-reviewed medical and scientific journals and have been awarded more than $60 million in competitive grant funding. Over the past 20 years a total of eight clinical staff have received Order of Australia honours for their work. More at www.kids-cancer.org or www.schn.health.nsw.gov.au