The Commonwealth Government together with Minderoo Foundation today announced funding of $67 million to expand the internationally recognised Zero Childhood Cancer personalised medicine program (ZERO) - ensuring all Australian children and young people diagnosed with cancer are given the greatest chance of survival.
Cancer is the most common cause of death from disease in children in this country. Every year in Australia almost 1000 children and young people are diagnosed with cancer. The challenge in curing them all is that each child and each cancer is unique, meaning standard therapies are not effective for every child.
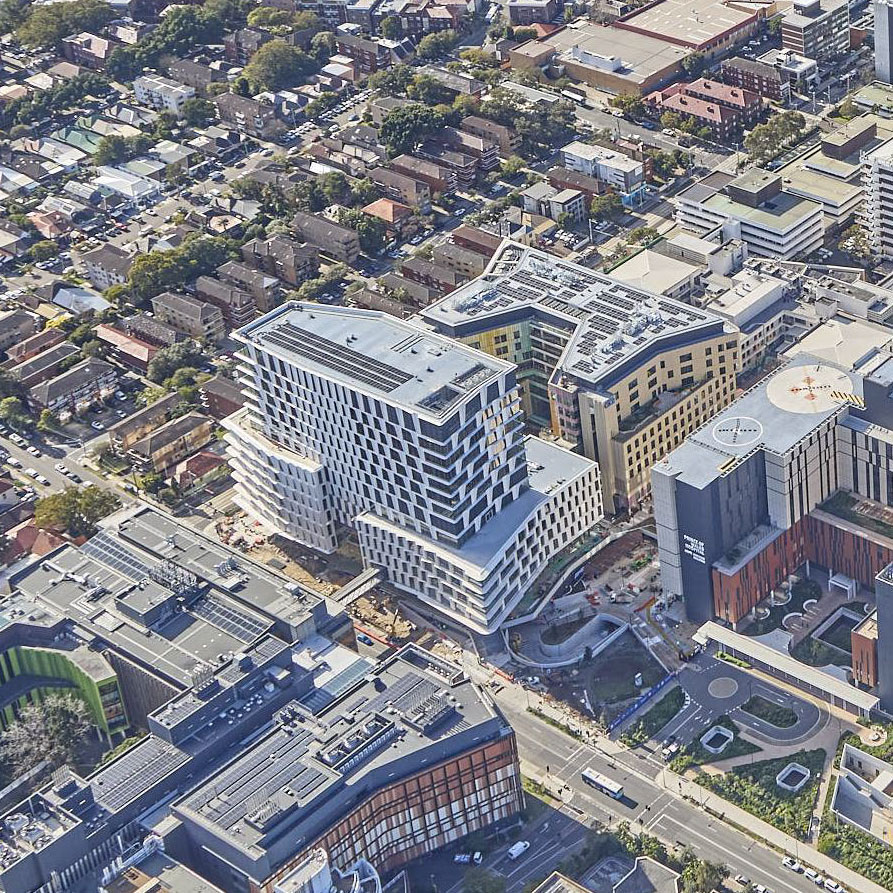
Led by the Children’s Cancer Institute and Sydney Children’s Hospital, Randwick, ZERO is only currently available to children across Australia diagnosed with the most aggressive cancers, or who have relapsed with less than 30% chance of survival. Today’s funding announcement by the Commonwealth Minister of Health, the Hon Greg Hunt, of $54.8 million from the Federal Government and $12.2 million from Andrew and Nicola Forrest’s Minderoo Foundation, will extend the genetic testing of the ZERO program to all Australian children diagnosed with cancer, by 2023.
The ZERO program’s extremely comprehensive genetic analysis, combined with pre-clinical drug testing, allows its team of clinicians and scientists to identify the drugs most likely to kill each child’s individual cancer, when standard treatments have failed. The world-leading ZERO approach identifies new personalised treatments that may afford each child the greatest possible chance of survival and quality of life.
This funding will mean all Australian children will have access to the program at the time of diagnosis, whereas today many of the children on the national ZERO trial will have relapsed after receiving standard therapy and this can mean finding effective new treatments is more challenging. By enabling all children access early in their cancer journey, the program aims to reduce the chance of relapse.
According to Professor Michelle Haber AM, Executive Director of Children’s Cancer Institute, this means “through this phased expansion of ZERO over the next three years, every child in Australia who is diagnosed with cancer will have access to personalised treatment recommendations that aim to give them the greatest chance of surviving their disease; ZERO also helps to identify less toxic targeted treatments reducing their risk of side effects,” she said.
In addition to providing access to ZERO for all Australian children with cancer, the funding boost will support the development of a comprehensive genomic databank of each patient’s healthy and cancer cells. This unique database will allow researchers to better understand the causes of childhood cancer, identify genetic markers that may be able to predict those at risk of the disease, and increase the ability to make better informed treatment recommendations.
Nowhere does this innovation mean more than on the hospital wards where kids with cancer are treated, A/Professor Tracey O’Brien, Director of the Kids Cancer Centre at Sydney Children’s Hospital, Randwick explains “every time you have to tell parents that treatment has failed and there is little hope of cure it is devastating. By working closely with researchers in the labs, our doctors are driving new ways of thinking, discovering new treatment options, and giving renewed hope for survival and a better future for kids with cancer. Zero deaths is our goal and we won’t stop until we achieve it”.
Built on a collaborative network of all eight children’s hospitals in Australia and 22 international research partners, the first ZERO national clinical trial for children with aggressive cancer was launched in September 2017. The results have been remarkable with over 300 children enrolled, and potential personalised treatment recommendations made for more than 70% of the children, which are now being reported to the children’s treating doctors within eight weeks on average. For the first group of children with clinical follow up who have received the recommended treatment plans, 50% have had a complete or partial response, or their disease has been stabilised. In addition, the findings from ZERO have led directly or indirectly to the opening of 23 new clinical trials for children with cancer in Australia.
The impact of Zero Childhood Cancer is demonstrated through stories like that of 15-year-old Kaylee who was diagnosed with stage 4 neuroblastoma in 2018, with tumours found throughout her body. For 18 months she was given every treatment possible – none of which proved effective. In mid- 2019 her oncologist discovered that Kaylee’s tumours had begun to grow rapidly and she was enrolled in ZERO, where the genetic footprint of her tumours were tested and a specific mutation was discovered in her tumour’s DNA. Lorlatinib, a drug typically used to treat lung cancers, was identified in the laboratories to possibly help target Kaylee’s specific cancer cells. While treatment is ongoing, Kaylee explains that “every child deserves something like this, it’s so needed and it makes everything so much easier, it works like a miracle”.
ZERO is changing the model of care for children with cancer by identifying new treatments specifically targeted to each child’s individual cancer and facilitating access to the right drug for the right child at the right time.
Key facts:
• ZERO has established Australia as an international leader in paediatric precision medicine. It is the leading childhood cancer program that is delivering integrated whole genome sequencing, whole transcriptome sequencing and methylation profiling to improve treatment and clinical outcomes in real-time.
• ZERO has not only led to improved outcomes for the children with aggressive cancer on the first national clinical trial, but has identified a high level of germline cancer predisposition in these children. In the future this could help to predict a child and their family’s susceptibility to developing cancer.
• ZERO is only at the beginning of this paradigm-shifting journey. Having established a national platform for the small proportion (~20%) of paediatric cancer patients with the most aggressive cancers, the program has already shown that with these technologies, it is possible to explain the molecular basis of the vast majority of child cancers and identify potential treatment options for 74% of patients. Early data demonstrates remarkable rates of response to genomically-guided individualised targeted treatments in children with high-risk disease
• Beyond investigating clinical impacts, large-scale discovery programs like ZERO are vital resources driving expansion of workforce capabilities to meet the new demands of precision medicine guided care, and the discovery of new targets and pathways important in child cancers. ZERO is identifying new treatments not currently available to children and facilitating access to the right drug for the right child at the right time.
• A further critical benefit of ZERO for children with cancer is the sharing and accessing of child cancer data globally. ZERO will develop novel data systems, integrating clinical, sequencing and other research data to improve precision medicine recommendations. This will also facilitate global sharing of these data and discoveries to maximise the net positive return on research investment.